Ask Our Experts
The silver lining of an incidental cancer diagnosis
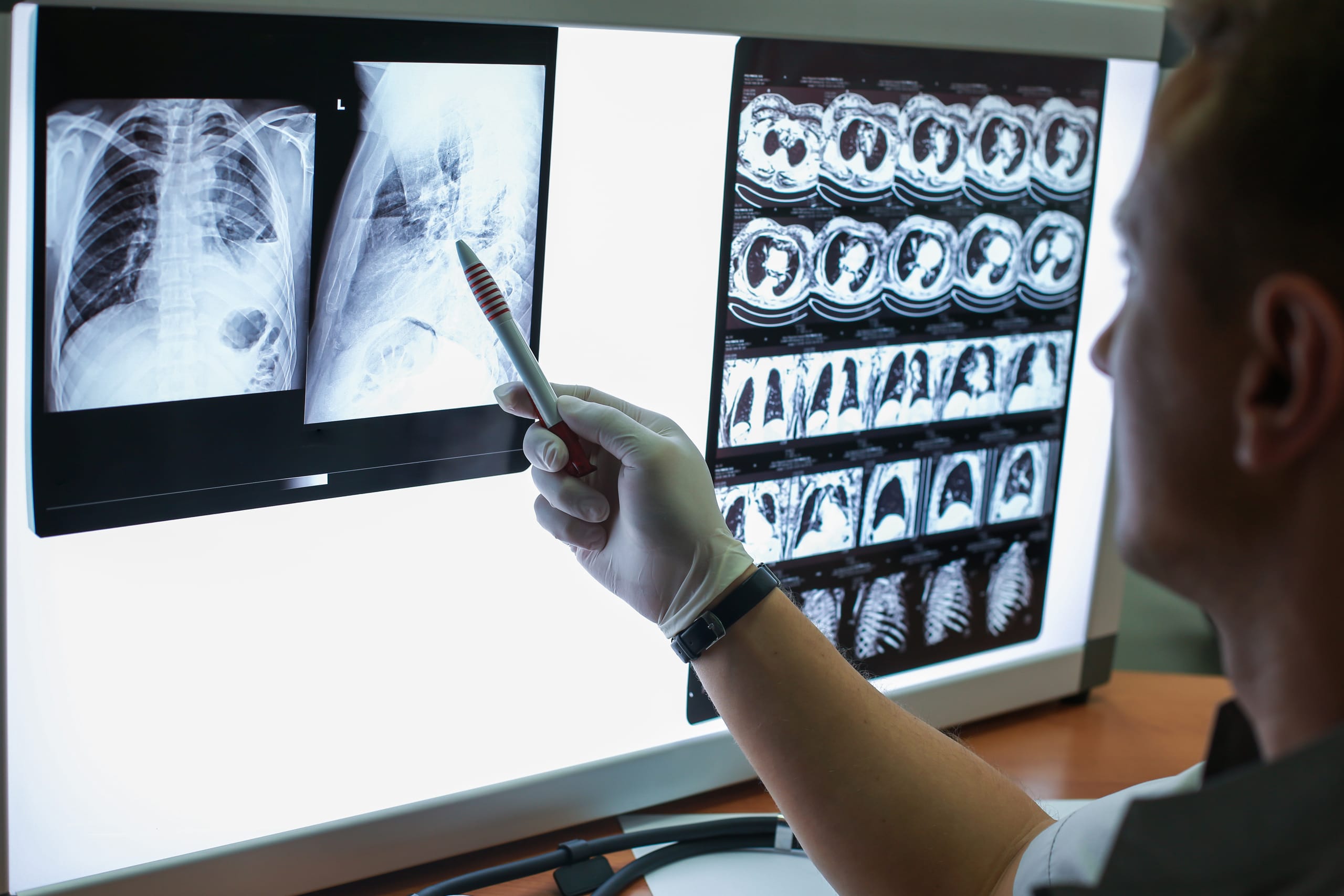
It’s a frightening thought. You’ve fallen off a bike and injured yourself, but the scan that was supposed to assess for damage to the ribcage discovered a mass in your right lung. Suddenly, a painful bone is no longer the most pressing concern. Could this unexpected mass be cancer?
This is what’s called an incidental finding. A test was done for one reason, but it picked up something different. Incidental findings are fairly common. Chest CTs result in them about 45% of the time1. With brain and spine MRIs, they occur about 22% of the time2. For combined imaging tests, the figure is about 24%3.
Of incidental findings, about half are recommended for follow-up4,5, and of those, the percentage that end up being cancerous varies by body location. Suspicious incidental findings in the breast are cancerous about 40% of the time. In the ovaries, thyroid, and kidneys, it is 25% of the time, and in the colon or prostate, about 15% of the time2. But altogether, only ~10% of incidental findings are malignant2,5. Here at PHM, we have extensive experience assisting patients with incidental findings, including Larry, who was diagnosed with incidental gastric cancer.
How often is cancer diagnosis incidentally?
In the United States, about 70,000 people are diagnosed with cancer incidentally each year. This equates to about 4% of all cancer diagnoses6. However, the figure varies significantly across cancer types. Nearly 25% of leukemias are diagnosed incidentally, owing to routine blood tests. Other cancers more likely to be found incidentally include kidney (9% of total), lung (15%), and colorectal (13%). In these cases, they are often diagnosed either before or after an elective surgery or during investigations for unrelated clinical issues7.
An incidental diagnosis can have an upside
An incidental cancer diagnosis is shocking. The person often has experienced no symptoms but is now facing treatment that could involve surgery, radiation, and chemotherapy. These interventions significantly impact day-to-day life. And yet, there could be a silver lining.
Many cancers do not have robust screening protocols, including pancreatic, kidney, liver, lung, and others8. This means that many are only found when the tumor has spread and is causing noticeable symptoms. Indeed, overall, only about 25% of lung cancers are detected when the tumor is early stage, when treatment is much easier and more successful9. On the other hand, if lung cancer is detected incidentally by a CT scan, these numbers are inverted—approximately 70% are stage I, which equates to a much better outcome10. And this pattern is similar with other cancer types11-13.
Should more frequent imaging be standard procedure?
If incidental cancer discovery is linked to better outcomes, why not do frequent imaging screenings in the hopes of finding these cancers early?
It is a difficult question because there are also downsides to extensive imaging. Frequent surveillance imaging is likely to identify many lesions of unknown significance. When this happens, it can lead to a cascade of tests, doctor’s visits, and interventions that can be invasive and ultimately, unnecessary. This can cause intense stress, strained social relationships, and financial difficulty14-16. For example, imaging may identify pre-cancerous lesions that are of indeterminant concern, and the medical advice is to “wait-and-see”. They may never progress, but waiting and not knowing if they will ever grow can cause crippling anxiety that triggers the need for additional interventions to address mental health17. In fact, many incidental findings end up being benign growths or false alarms that never would have caused a clinical issue.
In the future, rational screening approaches that can identify early cancer with more precision will be more widely available. One example is non-invasive tests that detect the presence of microscopic cancer in the blood8. The goal of these is to find cancer prior to any symptoms but also eliminate findings of unknown significance that can cause anxiety. If this is accomplished, the downside of more frequent screening could be eliminated.
What should I do if an incidental finding arises on my imaging?
While these findings are distressing, it is important to remain calm and try to proceed as methodically as possible. The first step is to verify the result. Ensure your primary care physician, specialists, and radiologist reach a consensus on what it could be. Also, consider having a second or third radiologist read the scan to see if they come to the same conclusion.
With multiple perspectives in hand, discuss the pros and cons of follow-up with your primary doctor. The decision for follow-up should incorporate three main factors:
- The likelihood of a serious finding that could get worse if left alone, making treatment more difficult in the future
- Your tolerance for anxiety while various tests and appointments occur
- The possibility of diagnosing something that may never have caused any clinical issues, leading to overtreatment and unnecessary side effects
Often, there is not one correct answer. The decision is a delicate balancing act between the patient, their family, and their doctors.
Finally, if a diagnosis of incidental cancer is made, it is important to process the information with a support network. Sometimes, it can be helpful to remember that if it had not been found incidentally, it may have been worse when it was finally caught. And this means you may have gotten an early jump on treatment. This was the case with Larry. There is no regular screening for gastric cancer and finding the aggressive tumor early almost certainly saved his life. At PHM, we aim to support patients with incidental findings by providing detailed education and recommendations, locating the top experts to confirm the diagnosis, and helping to guide through follow-up tests and treatment – ensuring the best possible care and outcome.
References
- Shaughnessy, A. F. Incidental Findings Are Common with Chest CT and MRI of the Spine and Brain. Am Fam Physician 98, 682 (2018).
- O’Sullivan, J. W., Muntinga, T., Grigg, S. & Ioannidis, J. P. A. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ 361, k2387, doi:10.1136/bmj.k2387 (2018).
- Lumbreras, B., Donat, L. & Hernandez-Aguado, I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol 83, 276-289, doi:10.1259/bjr/98067945 (2010).
- Mabotuwana, T., Hombal, V., Dalal, S., Hall, C. S. & Gunn, M. Determining Adherence to Follow-up Imaging Recommendations. J Am Coll Radiol 15, 422-428, doi:10.1016/j.jacr.2017.11.022 (2018).
- Gibson, L. M. et al. Potentially serious incidental findings on brain and body magnetic resonance imaging of apparently asymptomatic adults: systematic review and meta-analysis. BMJ 363, k4577, doi:10.1136/bmj.k4577 (2018).
- Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J Clin 69, 7-34, doi:10.3322/caac.21551 (2019).
- Koo, M. M., Rubin, G., McPhail, S. & Lyratzopoulos, G. Incidentally diagnosed cancer and commonly preceding clinical scenarios: a cross-sectional descriptive analysis of English audit data. BMJ Open 9, e028362, doi:10.1136/bmjopen-2018-028362 (2019).
- Liu, M. C. et al. Sensitive and specific multi-cancer detection and localization using methylation signatures in cell-free DNA. Ann Oncol 31, 745-759, doi:10.1016/j.annonc.2020.02.011 (2020).
- Blandin Knight, S. et al. Progress and prospects of early detection in lung cancer. Open Biol 7, doi:10.1098/rsob.170070 (2017).
- Quadrelli, S., Lyons, G., Colt, H., Chimondeguy, D. & Buero, A. Clinical characteristics and prognosis of incidentally detected lung cancers. Int J Surg Oncol 2015, 287604, doi:10.1155/2015/287604 (2015).
- Dall’Oglio, M. F. et al. Incidental and symptomatic renal tumors: impact on patient survival. Sao Paulo Med J 120, 165-169, doi:10.1590/s1516-31802002000600002 (2002).
- Kawauchi, D. et al. The clinical characteristics and outcomes of incidentally discovered glioblastoma. J Neurooncol 156, 551-557, doi:10.1007/s11060-021-03931-3 (2022).
- Takeda, Y. et al. Asymptomatic Pancreatic Cancer: Does Incidental Detection Impact Long-Term Outcomes? J Gastrointest Surg 21, 1287-1295, doi:10.1007/s11605-017-3421-2 (2017).
- Ganguli, I. et al. Cascades of Care After Incidental Findings in a US National Survey of Physicians. JAMA Netw Open 2, e1913325, doi:10.1001/jamanetworkopen.2019.13325 (2019).
- Bomhof, C. H. C. et al. The Impact of Incidental Findings Detected During Brain Imaging on Research Participants of the Rotterdam Study: An Interview Study. Camb Q Healthc Ethics 29, 542-556, doi:10.1017/S0963180120000304 (2020).
- Schmidt, C. O. et al. Psychosocial consequences and severity of disclosed incidental findings from whole-body MRI in a general population study. Eur Radiol 23, 1343-1351, doi:10.1007/s00330-012-2723-8 (2013).
- Xu, J., Neale, A. V., Dailey, R. K., Eggly, S. & Schwartz, K. L. Patient perspective on watchful waiting/active surveillance for localized prostate cancer. J Am Board Fam Med 25, 763-770, doi:10.3122/jabfm.2012.06.120128 (2012).
