Feature Article
COVID-19 Vaccines on The Horizon
Private Health is closely monitoring the development of COVID-19 vaccines to help our clients understand the latest announcements and make the best choices for the health and safety of their families.
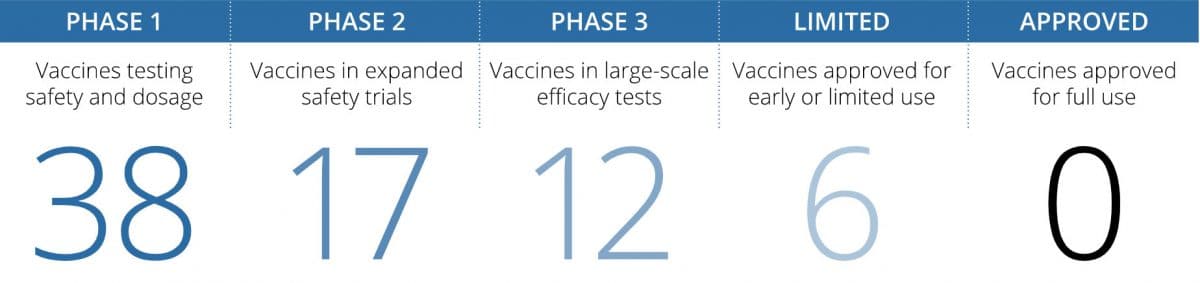
The recent news from Pfizer (in partnership with BioNTech) and Moderna that their vaccines are preventing approximately 95% of symptomatic COVID-19 infections, and that the vaccine from AstraZeneca (in partnership with the University of Oxford) showed between 62-90% efficacy (depending on the dose given) is very promising. And these are just three of the dozens of vaccines currently being tested in humans, making it highly likely that several effective vaccines are on the horizon. These breakthroughs provide our best hope to curb the virus in 2021, allowing us to begin the social and economic recovery in the coming months, not years.
Once more complete data is released, Private Health’s research department will study each FDA authorized vaccine in detail to determine if we recommend one vaccine over another in general or for a specific population. For example, certain vaccines may be a better fit for children, older adults or individuals with certain underlying health conditions.
The vaccine landscape is changing almost daily, but here’s Private Health’s current perspective on some key questions:
1. Given the recent Pfizer, Moderna, and AstraZeneca announcements on the success of their vaccine trials, when do we think vaccines might be available to the public?
Global Supply
Pfizer expects to produce up to 50 million doses of its vaccine in 2020 and up to 1.3 billion doses in 2021 globally. Moderna expects to have 20 million doses of its vaccine ready to ship in the US by the end of the year and to manufacture between 500 million and one billion doses in 2021. AstraZeneca expects to produce up to three billion doses in 2021. Keep in mind that only a portion of the global vaccine production will be allocated to the U.S. and that these vaccines require two doses for immunization, meaning that 50 million doses would immunize 25 million people. Other vaccine manufacturers are likely to follow fast on the heels of this success and will likely add to the global supply.
Who Will Receive the Vaccine and When
A clear distribution plan is yet to be released, and there remain many unknowns regarding who will receive the vaccine, how, and when. We anticipate that Emergency Use Authorization (EUA) for the Pfizer (and possibly Moderna) vaccine may be granted as early as December of 2020, and some distribution will begin immediately. Pfizer submitted their application on November 20, 2020. Certain populations (e.g., healthcare workers, the elderly, those with underlying medical conditions, some essential workers) will likely receive priority access to vaccines. We anticipate that the general public will begin to receive these vaccines sometime in 2021.
Factors that May Delay Vaccine Distribution
There may be unexpected delays in vaccine distribution due to challenges in cold-chain management, distribution channels, vaccine tracking, safety and efficacy monitoring in the real world, and/or manufacturing. A note on manufacturing – while mRNA vaccines (like those of Pfizer and Moderna) are expected to be more scalable than traditional vaccine platforms, making them excellent candidates for a “quicker fix” to a global pandemic, they may still be affected by manufacturing hurdles or manufacturing-related FDA holds that ultimately cause distribution delays.
2. How have Pfizer and Moderna been able to achieve over 90% efficacy when previous standards are much lower? Can we trust the results?
The Current State
The reported efficacy of Pfizer’s and Moderna’s vaccines are nearly equivalent, both with around a 95% rate of prevention from symptomatic disease in clinical trials. The seasonal flu vaccine, by comparison, is <60% effective. One of the possible reasons for such high efficacy of the two COVID-19 vaccines is the use of a novel mRNA platform which is fundamentally different from traditional vaccine platforms. No mRNA vaccine has ever been authorized by the FDA before. Clearly, these COVID-19 mRNA-based COVID-19 vaccines are already showing great promise, and the high efficacy read-out came as a welcome surprise to many. The FDA had set their efficacy threshold at 50%, and the Pfizer and Moderna vaccines have impressively surpassed that requirement, signaling that their path to EUA, and eventual approval, may happen quickly.
Translating Clinical Trial Results to Real World Data
It’s important to remember that the ~95% figure reported by Pfizer and Moderna is a clinical trial readout and does not necessarily reflect the vaccines’ effectiveness in the real world. Efficacy of a vaccine in a clinical trial can differ from its real-world effectiveness when the conditions and/or populations studied in the clinical trial do not perfectly represent the real world. For example, clinical trial populations may differ from the general population in many ways, including socio-economic status, race, absence of certain underlying medical conditions, etc. As a result, while the 95% efficacy reported in clinical trials is extremely promising, it may not be as high as this in the general population.
Interpreting the Efficacy Data
In order to determine a vaccine’s efficacy, a large population is enrolled in a clinical trial, and some are given the vaccine while others are given placebo. Once a certain number of people become symptomatic with COVID-19 (in Pfizer’s case, the company waited until 170 people became infected; Moderna waited until they had 95 confirmed cases), the company determines how many of those sick people were vaccinated and how many were not. In Pfizer’s case, 162 people who became sick received placebo and only 8 people who became sick received the vaccine; in Moderna’s case, 90 of the 95 infected people received placebo and 5 received the vaccine. The company then compares the rate of infection in the vaccinated group to the rate of infection in the placebo group – this is known as efficacy, reported by Pfizer as 95% and Moderna as 94.5%.
Trustworthiness of the Clinical Trial Data
We believe that the clinical trials run by both Pfizer and Moderna adhered to the high standards of clinical trial design and data analysis that we have come to expect from pharmaceutical companies seeking drug approval in the U.S. While the detailed data has not yet been formally published in an academic journal, the companies will be presenting it to a panel of experts who will determine whether EUA will be granted. Eventual FDA approval will likely follow, assuming continued positive data for efficacy and safety.
Additional Questions Remain
The data so far suggests that immunization delivers a favorable immune response, protection from symptomatic disease, and a favorable safety profile. However, additional questions remain:
- Does protection vary by subpopulation (e.g., age, race, clinical conditions)?
- Does the vaccine protect against re-infection, or do vaccinated individuals get re-infected but remain asymptomatic?
- What is the durability of protection (i.e., does it wane) and how long does protection last?
3. How does the AstraZeneca vaccine compare to the Pfizer and Moderna vaccines?
Is it as good?
Different Technology Unlike Pfizer and Moderna’s vaccines, which use mRNA technology, AstraZeneca’s COVID-19 vaccine uses a different technology called a viral vector. While no other vaccines using this technology have yet been approved for human use, some viral vector vaccines are approved for use in animals.
Efficacy
So far, AstraZeneca has analyzed data from a total of 11,636 participants, showing an overall efficacy of 70%. However, this analysis combines the results from two different groups, who each received different doses of the vaccine. When analyzed separately, one group, given two full doses a month apart, saw an efficacy of just 62%, while the other group, who was given an initial half dose followed by a full dose a month later, saw an efficacy of 90%. This second dosing strategy, which has the added advantage of using less vaccine per person and thus will enable vaccination of more people globally, appears to have efficacy approaching that of the Pfizer and Moderna vaccines.
Distribution
The AstraZeneca vaccine can be stored and transported at normal refrigerated temperatures. This contrasts with the Pfizer and Moderna vaccines, which require colder temperatures for transport and long-term storage.
4. Do we know how long the vaccines will provide protection?
The durability and duration of protection from COVID-19 vaccines remains unknown. Different vaccines could ultimately provide different levels of protection; these questions will not be resolved until long-term data from all the vaccine trials is available. We anticipate that after the first two initial doses, a booster shot may be required, potentially annually.
5. What do we know so far about how vaccines will be distributed?
It isn’t enough for a vaccine to be effective, it must also be efficiently delivered and widely adopted. Distribution of COVID-19 vaccines presents an unprecedented challenge given the scale of the present pandemic. Distribution will not begin until EUA for any particular vaccine is granted, which can happen as early as December for the Pfizer (and possibly Moderna) vaccine. The CDC has drafted its “COVID-19 Vaccination Program Interim Playbook for Jurisdiction Operations,” which provides guidance on vaccine distribution for states, territories, and local governments. Allocation and distribution will vary in all jurisdictions, depending on the priorities and specific populations in any given community. It will be important to check with your local health authority to find out more details.
Phased Roll-Out of Vaccines
The CDC predicts that vaccine rollout will proceed in three phases:
Phase 1
A short period of time over which vaccine supply is limited and doses are prioritized for certain groups with inventory tightly controlled. Priority is expected to be given to paid and unpaid healthcare workers who are at risk of COVID-19 infection, other essential workers (e.g., emergency and law enforcement personnel, food packaging and distribution workers, teachers/school staff, childcare providers, etc.), and people at higher risk for severe COVID-19 illness due to underlying medical conditions, including those over the age of 65. During this time, distribution channels will be limited to those best suited for reaching these populations (e.g., large hospitals).
Phase 2
Supply increases and access expands to include additional critical populations as well as the general population. These are expected to include additional critical infrastructure and essential workers not vaccinated in Phase 1 (e.g., vaccinators, pharmacy staff, ancillary staff, school nurses, EMS providers, security personnel, etc.), those at increased risk of acquiring or transmitting COVID-19, those with limited access to routine vaccination services, as well as the general public. Distribution channels will expand to a broader set of providers including pharmacies, clinics, doctors’ offices, public health sites.
Phase 3
Supply is sufficient and there is open access to vaccines across populations, including the general public. Vaccines are integrated into routine vaccination programs. Networks for distribution broaden and include private partner sites.
There may be initial age restrictions for vaccine products, depending on the data available from clinical trials.
Vaccine Allocation
The federal government will allocate the vaccines taking into account multiple factors, including:
- Critical populations recommended by the Advisory Committee on Immunization Practices (with input from the National Academies of Sciences, Engineering, and Medicine)
- COVID-19 vaccine production and availability
- Overall population of the jurisdiction
Distribution Channels
Most likely, the distribution channels in Phase 1 of vaccine rollout will be limited, tightly controlled, and intended to exclusively serve the prioritized populations. In Phase 2, additional distribution channels/providers are expected to begin participating in vaccine administration. To maximize access to COVID-19 vaccines for all Americans, the U.S. Department of Health and Human Services (HIS), announced a partnerships with large chain pharmacies and networks that represent independent pharmacies and regional chains. By working with these partners, the federal government will rapidly expand access to COVID-19 vaccines at no cost to patients. We expect pharmacies, such as CVS Health, will begin administering vaccines once Phase 1 populations have been served.
As soon as vaccines are available, Private Health will facilitate access to our clients however possible.
6. Have the trials included enough people of different ages, races and underlying conditions to be considered safe broadly?
Even after receiving EUA from the FDA, vaccine studies will continue for the next two years to evaluate ongoing safety and efficacy across the real population. There is still much to learn on the question of representation in the clinical trials, but we do have some early indication directly from the companies.
In Moderna’s trial, the 95 cases included 15 people 65 or older and 20 people who were Hispanic, Black, Asian or multiracial (source: Moderna press release).
In Pfizer’s trial, approximately 42% of global participants and 30% of U.S. participants have racially and ethnically diverse backgrounds, and 41% of global and 45% of U.S. participants are 56-85 years of age (source: Pfizer press release and Pfizer).
In AstraZeneca’s trial, the 23,000 participants assessed so far include individuals who are over 18 years of age from diverse racial group and geographic regions, who are healthy or have stable underlying medical conditions (source: AstraZeneca press release).
